Pre-diabetes
The Facts about
the A1c Test

What is an A1c Test?
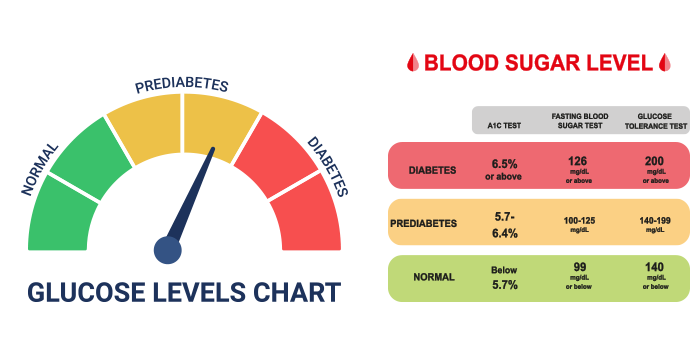
The A1c test (also known as the glycated hemoglobin, glycosylated hemoglobin A1C or HbA1c test) is a blood test that measures how much sugar is attached to your blood’s hemoglobin protein. The test gives a measurement of how well your body has controlled the amount of sugar in your bloodstream over the past 2-3 months.
Knowing your A1c levels is the first step to understanding if you are prediabetic or have diabetes.
What is pre-diabetes?
Pre-diabetes is defined as a higher than normal blood sugar level in the body. This elevated level is not high enough to be classified as type 2 diabetes, but it can quickly develop into type 2 diabetes in adults and children without dietary and lifestyle changes.
What are the health risks of pre-diabetes?
The long-term damage of diabetes to your organs–especially your heart, blood vessels, and kidneys–can start during pre-diabetes. Pre-diabetes has been linked to silent heart attacks. The good news, however, is that progression from pre-diabetes to type 2 diabetes is not inevitable. If you reverse weight gain, stay at a healthy weight, eat healthy foods, and get regular exercise, you can bring your blood sugar level back to normal.
What are the symptoms of pre-diabetes?
Possible symptoms of pre-diabetes or signs that you have moved from pre-diabetes to type 2 diabetes, include:
- Darkened skin on certain parts of the body: neck, armpits, and groin areas
- Increased thirst
- Frequent urination
- Increased hunger
- Unexpected weight loss
- Blurring vision
- Feelings of general and persistent fatigue
- Numbness and/or tingling in the hands or feet
- Frequent infections
- Slow-healing sores
- Unintended weight loss
Contact your healthcare provider if you have any of the above symptoms or if you are concerned about possible pre-diabetes and want to have a blood sugar screening test.
What are the causes of pre-diabetes?
The exact causes of pre-diabetes are not known, but family history, genetics and lifestyle choices all appear to play a critical role. What is known definitively is that people with pre-diabetes do not process glucose (sugar) properly anymore.
What is glucose?
Glucose is a simple sugar which is a component of many carbohydrates and an important source of energy.
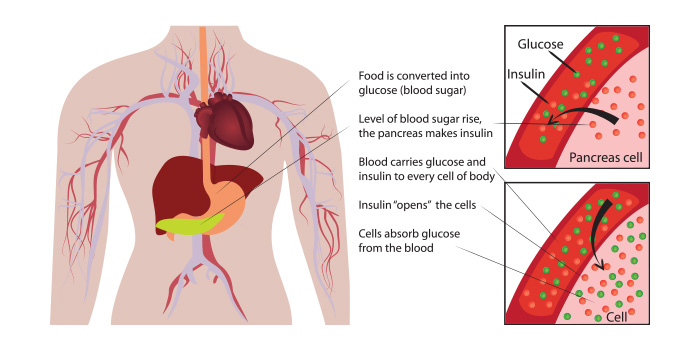
Most of the glucose in your body comes from the food you eat. When food is digested, sugar enters your bloodstream. Insulin, an enzyme produced by your pancreas, lowers the amount of sugar in your blood by helping sugar enter your cells where it is used as energy.
Your pancreas automatically sends insulin to your blood when you eat. The amount depends on how much sugar is present. When your blood sugar level starts to drop, the pancreas slows down the secretion of insulin into the blood.
When you have pre-diabetes, this process does not work as well as it should. Sugar, instead of entering and fueling your cells, builds up in your bloodstream.
This breakdown might happen because:
- Your pancreas may not be making enough insulin
- Your cells have become resistant to insulin and don’t allow as much sugar in
Understanding how insulin works
What are the greatest risk factors for developing pre-diabetes?
The same factors that increase the chances of getting type 2 diabetes also increase the risk of pre-diabetes. These factors include:
- Weight. Being overweight is a primary risk factor for prediabetes. The more fatty tissue you have, especially inside and between the muscle and skin around your abdomen, the more likely your cells will become resistant to insulin.
- Waist size. A large waist can indicate insulin resistance or an increased risk for pre-diabetes. Men with waistlines larger than 40 inches and women with waistlines larger than 35 inches are at greater risk.
- Diet. Drinking sugar-sweetened beverages and consuming large quantities of red meat can create a higher risk of pre-diabetes.
- Inactivity. The less active you are, the greater your risk of pre-diabetes.
- Age. Diabetes can develop at any age, but the risk of prediabetes increases after the age of 45.
- Family history. Having a parent or sibling with type 2 diabetes increases your risk.
- Race or ethnicity. Black, Hispanic, American Indian, and Asian American people are more likely to develop pre-diabetes.
- Gestational diabetes. If you had diabetes during a pregnancy (gestational diabetes), you and your child are at higher risk of developing pre-diabetes.
- Polycystic ovary syndrome. If you have irregular menstrual periods, excess hair growth, and obesity, you are at greater risk.
- Sleep. Obstructive sleep apnea, a condition that disrupts sleep repeatedly, creates a greater risk for insulin resistance. People who are obese or overweight are more likely to develop obstructive sleep apnea.
- Tobacco smoke. Smoking may increase insulin resistance and can increase the risk of type 2 diabetes in people with pre-diabetes.
- High blood pressure. High blood pressure is often called the silent killer because it can damage your kidneys, brain, heart and other organs without you noticing symptoms. It also increases your risk of pre-diabetes.
- Low levels of high-density lipoprotein (HDL) cholesterol. Low levels of this “good” cholesterol increases risk of prediabetes
- High levels of triglycerides. This type of fat in your blood in high levels also increases risk of pre-diabetes.
Metabolic syndrome
When certain medical conditions occur alongside obesity, these conditions can contribute to insulin resistance, and can increase your risk for diabetes, heart disease, and stroke. A combination of three or more of these conditions is often called metabolic syndrome:
- High blood pressure
- Low levels of HDL
- High triglycerides
- High blood sugar levels
- Large waist size
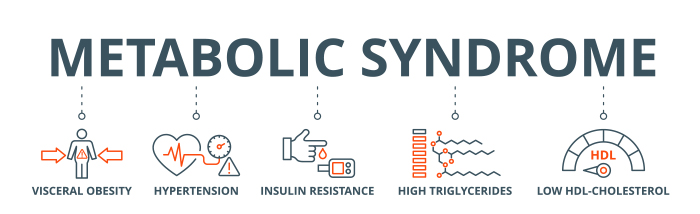
Exercise, weight loss, a healthy diet, smoking cessation, and often medications can help reverse the health dangers of metabolic syndrome.
What are the health risks if pre-diabetes develops into type 2 diabetes?
If pre-diabetes progresses to uncontrolled type 2 diabetes, the health risks are serious, including:
- High blood pressure
- High cholesterol
- Heart disease
- Stroke
- Kidney disease
- Nerve damage
- Fatty liver disease
- Eye damage, including loss of vision
- Amputations
How can I prevent pre-diabetes and its progression?
Even if diabetes runs in your family, you can take lifestyle steps that can help you prevent pre-diabetes. These include:
- Eating healthy foods and avoiding highly processed foods and meats
- Staying physically active
- Losing excess weight
- Stopping cigarette smoking if you currently smoke
- Controlling your blood pressure and cholesterol level

At LifeStyle Medical Center, our team of professionals is focused on long-term dietary and lifestyle changes that prevent type 2 diabetes and other chronic diseases. Remember, progression from pre-diabetes to type 2 diabetes is not inevitable. If you reverse weight gain, stay at a healthy weight, eat healthy foods, and get regular exercise, you can bring your blood sugar level back to normal.
Are you ready to start down the path to a healthier you?
Reverse pre-diabetes?
Take control of your health today. Better health IS within your reach.
Take the first step today. Call us today @ (919)354-7077
Sources:
- Centers for Disease Control and Prevention, https://www.cdc.gov/.
- Mayo Clinic, https://www.mayoclinic.org/.
- Johns Hopkins Medicine, https://www.hopkinsmedicine.org/health.
- Cleveland Clinic, https://my.clevelandclinic.org/health/diseases.
